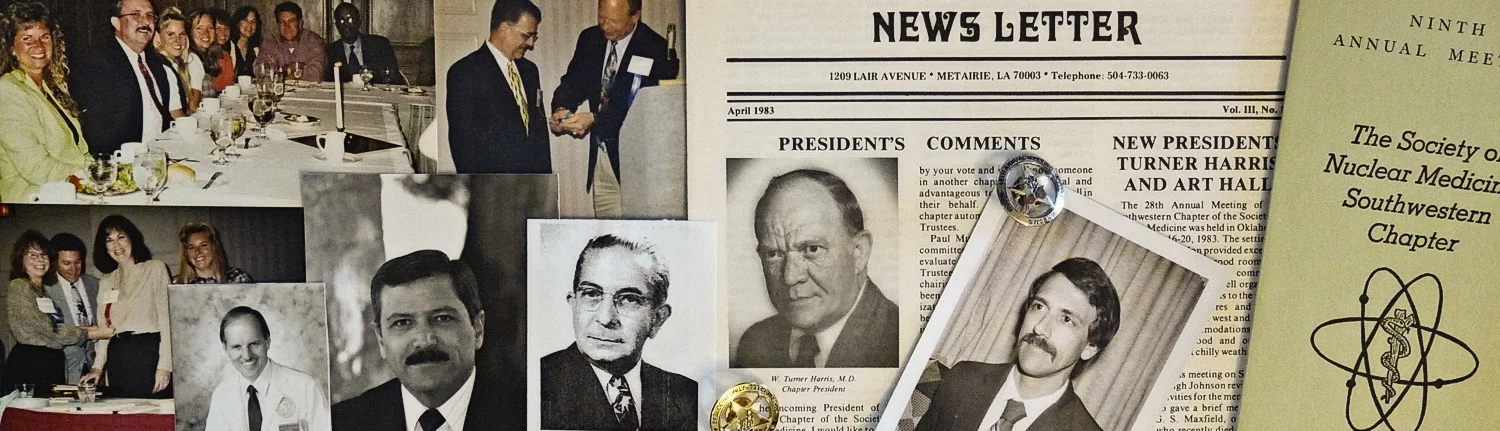
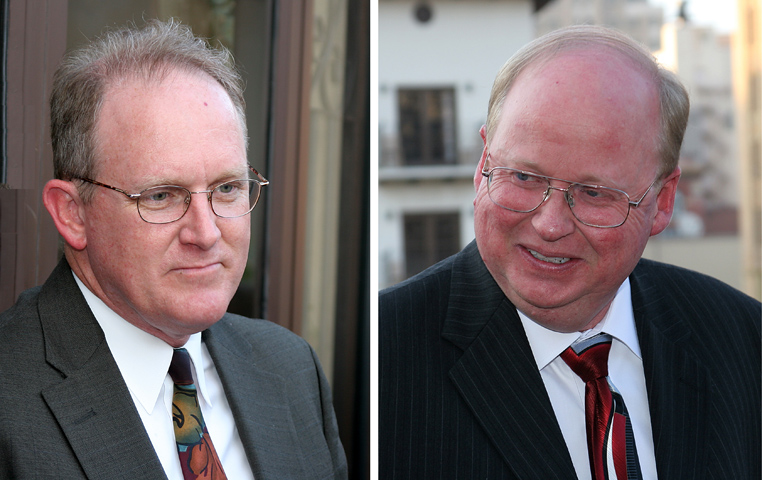
John Pickett (left) and Glenn Smith (right)
14th and 15th Presidents of the SWCSNM-TS.
2005 CONFERENCE CALL BETWEEN JOHN PICKETT and GLENN SMITH (both past Technologist Section Presidents)
MR. PICKETT: Well, I just want to clear up that Martha Pickett and John Pickett are not related.
MR. SMITH: That was something people would frequently ask, and I think that's one of the first things you told me—that you and Martha were not married.
MR. PICKETT: Right, we're not married. She lives in Arkansas. We're not even related.
I actually have a funny story about that, though. One year at a Chapter meeting, they tried to put Martha in my room. She was checking in, and they were going to put her in John Pickett's room. Now, my wife's name is Barbara, and we had a good laugh about that—Martha, my wife, and I. Barbara and Martha have met and they know each other, and it's just been funny over the years.
MR. METZGER: John, how did you first become involved with Chapter leadership?
MR. PICKETT: Well, like many have experienced, if you volunteer to become involved, you are quite likely to be appointed to some committee or nominated for election. Back in the early '80s, I volunteered, and I think I was placed on some committee (I don’t recall which one).
I was program chairman, I believe, in '84, and then ran for president in '85/'86, but you had a handful of maybe 10 or 12 active people each and every year. And it was hard to get people involved. You pulled upon the people that you knew, and most people shied away because it was going to be extra work or whatever. But actually, it wasn't that much extra work, and it was pretty enjoyable.
It was an honor to get to work for the Society, especially in those years because those were fledgling years. We were really struggling. Nuclear medicine as a whole was struggling after DRGs (Medicare’s Diagnosis Related Groups). DRGs were being imposed and changed the rules, and in 1983 or 1984, the practice of nuclear medicine changed dramatically—almost overnight. Glenn, you were educating then too, weren't you?
MR. SMITH: Yes, and it caught up with us and our college budget a couple years later, and that really cut back on the traveling money. At one of our meetings, I still remember a girl standing up and just about in tears saying, “Look at the money that we've generated for the hospital over all these years, and it doesn’t matter anymore.”
What mattered was what you, as the patient, went in with, was what you received in funds to cover your hospital stay. The more procedures you did, the less money the hospital made, so they (omit –had) really cut back. Education always takes two years to catch up, so two years later our enrollments went down because of the impact of DRGs. But, you know, just like everything, the practice of nuclear medicine goes in cycles, and if you don't make it per procedure, they figured out, we'll make it per patient volume, and then they started hiring people back again.
MR. PICKETT: To get back to the leadership question: Art Hall was president two years before I was, and because we both worked for the same company (Numed), Art was my inspiration to become more involved with the Chapter. Eventually, Art moved farther into the higher echelon of the National Society.
Art and the president of our company, then Ed Menkemeller, had always been very, very supportive. He’s deceased now, but he always sent all of our technologists to the Chapter meetings. He paid their way and was very, very supportive of education and of the Chapter. And that support continues on today. Ed passed away a couple of years ago, but he was always instrumental. He gave Art and me whatever time we needed. We didn't have to take off on our own. And especially with Art getting more involved at the National level, that was very generous.
MR. SMITH: John, if I remember right, back then you got accelerated into your president position too because the person that was supposed to serve went into sales or something and you immediately became president. Is that right?
MR. PICKETT: That’s true. I was president-elect and became president right away because Paul Yurko did not serve his term.
MR. SMITH: That's what I was thinking because even though I won some other position, you ended up nominating me as president-elect because you had to get someone to fill-in quickly. I think I might have been the Houston local rep to the Southwestern Chapter, and you nominated me because the meeting the next year was going to be in Houston and it helped to have somebody in town.
MR. PICKETT: I believe you're right about that. I was kind of thrown in the position, but it was a big help that Art had been the president two years before. He was able to help guide me.
MR. SMITH: I think he helped out just about everybody. He helped me in my presidency. And Brad Pounds was another one that was real active at that time. Brad and I were both active in the late '70s and the early '80s in the Houston area, and then Brad became active at the Chapter level (and later the National level). He helped me get interested in the Chapter and both Brad and Art helped out.
MR. PICKETT: At that point in time you didn’t just jump into the presidency. You served as program chairman or something else and then moved up. But as I said earlier, there was a group of 10 or 12 every year of pretty much the same people, except that they changed over the years. I mean, I dropped back, and Martha Pickett, Brad Pounds, and Sharon Ward—those folks became more involved, and everyone kind of served their duty in some way or another within the Chapter.
I need to add that the physician leadership—especially during my presidency and I assume every year since—was always very supportive of the technologists. They felt that the Technologist Section was a very important part of the Chapter and they supported the development of the technologist-oriented sessions at the meeting.
MR. METZGER: That's great. The positive support of the physician leadership has come up in a number of the interviews. And as I reviewed some interviews, I learned that it was the Southwestern Chapter that led to the development of the National Technologist Section.
MR. SMITH: That's what I've heard. Before he was associated with our school, our past medical director, Dr. Thomas Haynie and Gary Wood helped set up the National SNM Technologist Section. And let me tell you, Dr. Haynie is a super person. He worked as Houston Community College's medical director for years, and he was just an easy person to talk with. He would go to bat for you. He was just super supportive of us and the Society and is just an incredible person.
MR. PICKETT: Yeah. Physicians-wise, Bob Sonnemaker was the head when I was president, and he was extremely supportive of us, but there's lots of names to drop. Dr. Hightower, who was at Texas A&M, he was very supportive. And Dr. Petty was actually our mentor and put a lot of technologists out in the field. We had five technologists here graduate from Scott & White in Temple, Texas, and Dr. Petty ran that program.
He was president of the Chapter in the late '70s, and was very supportive of all of us students. He really pushed being in the Chapter and felt that was important. All those guys back then were like our elders. They were all extremely good leaders and very inspiring folks.
I have a story that tells you about the type of person Dr. Petty was. I had been a student at Scott & White for less than a week and was living in a trailer house here in Temple. Well, my father got very sick back in Amarillo. He was in the ICU back in Amarillo. And since we didn't have a phone yet, they called Scott & White to try to find me. Well, at some point, I look outside, and see Dr. Petty walking up and down the street out in the trailer park knocking on doors looking for me at the house, and about the same time the police showed up out there. Dr. Petty came to the neighborhood to try to find me, and I'm just a student of less than a week. That’s the type of man who was a leader of the nuclear medicine program here in Temple and also in the Chapter.
Marty Nusynowitz and a lot of these guys are those type of individuals in my opinion. They're just very high integrity-type guys and very compassionate and just good people. You give them their due respect, but they are just good folks.
MR. METZGER: Now, have you lived elsewhere? Because part of me thinks this is a Bible-belt reality. I'm not sure it's like that in Chicago and New York and San Francisco.
MR. PICKETT: I lived for six months in California when I was high school age. But otherwise I'm a native Texan from Amarillo when I was younger and now just north of Austin for the rest of my life.
MR. SMITH: That’s pretty much the same with me. I was born in Houston; we moved around quite a bit until I was a sophomore in high school. Ever since then, I've been in Houston, so I am a native Houstonian. In fact, the first place I worked in nuclear medicine was the place I was born—Hermann Hospital in Houston, Texas.
Before Hermann Hospital had a nuclear medicine section or department, I used to work for Dr. Herbert Allen, who did some of the first clinical nuclear medicine, and we used to have a contract with Hermann Hospital, and I'd walk bone scan doses across Fannin over into the building. So I thought that was a pretty good cycle—being born there and doing some of my first nuclear medicine in the same hospital.
John, you worked for Numed how many years?
MR. PICKETT: This is my 26th year.
MR. SMITH: Right. And I've been at Houston Community College (HCC) now going on 24 years, and my partner, Rene Hyder, has been with me for 23 years at the school, so it's pretty stable, I guess down here.
MR. PICKETT: That's true.
MR. METZGER: Glenn, how did you first get involved? What was your introduction to the Chapter?
MR. SMITH: Like I said, I was active in the Houston local society back in the late '70s, early '80s. Brad Pounds and I and a couple of other people pretty much ran the local group. We were pretty stable, except for 1981, which was the year that I started here at HCC and Brad became chief technologist at St. Luke’s. The local chapter disappeared for a year while we were getting used to our new positions, but then we both got active again and Brad helped me get involved at the Chapter level.
At some point, I became the local society’s representative to the Southwestern Chapter. After that, I got on committees, went to meetings, and that's how I got involved. And then John recruited me for the position of president-elect.
MR. METZGER: All right, and a question for both of you: .As you reflect on your years of leadership participation in the Chapter, what sort of highlights or accomplishments make you most proud?
MR. PICKETT: I was program chairman for the meeting which immediately preceded my presidency, and I look on that meeting as a highlight. I remember that Walter Durham did an excellent paper for us on I-131 therapy, and he was a guy of just really high regard within the Society. Everybody that knew him liked him. For that particular meeting, I just felt good about what we had as far as for the techs. I also remember Dave Campbell—who was chief technologist, I think—did a program on QC of SPECT, which was new. SPECT was new.
There just weren't a whole lot of SPECT cameras out there. Computerized tomography (CT) just kind of killed us on brain scans and took away all that business; so to have computerized tomography of nuclear medicine studies was quite new for a number of us. And David did a program on cell rotation and things that these kids nowadays all take for granted because they that's just part of their everyday work, but I just remember how interesting it was to me because it was all so brand new. Now we're 21 years down the road and that's just standard practice.
MR. SMITH: I can't remember if it was the year I was president or around one of those years. As I recall, our meetings were very well attended, but one of the things we were having problems with at that point was nobody was visiting our vendors in the exhibit halls. To remedy this, Brad Pounds and I came up with an idea about having a raffle in the halls. What would happen is the vendors would hand out tickets when you would go to visit the different booths, and it became a competition between the techs as far as how many tickets they could get to win the prizes at the end of the day.
That first year I asked for the prize donations; instead of being smart like they were in future years and asking the sales people for prizes, I went and solicited prizes in the Houston area, the Galleria, which was the mall that was next to where we were having the meeting. I called restaurants and shops to get dinners and gifts donated – I told restaurant and shop owners that we had all these doctors coming to the meeting, and I'm sure that they would be bringing their friends with them when they were redeeming their dinner or gift certificates, and I got quite a few prizes donated.
The raffle really did increase the number of visits that the vendors were getting, and that was important because the vendors were underwriting a lot of what we were doing at the time. I don’t think Brad could ever admit that he was one of the persons that thought up the raffle idea, because the doctor that was over where he worked at the time thought that was a tacky idea; that the raffle was like bribery and not such a hot idea. Yet I think it worked quite well.
MR. METZGER: Well, how about disappointments, failures, disasters, during your leadership years?
MR. PICKETT: I'm going to go back to 1984 and the Diagnosis Related Groups (DRGs). When DRGs came along, hospitals got a certain amount of money for a DRG for an inpatient being admitted. This is a different concept from the way it is nowadays. People hardly get hospitalized unless they're just really ill. Back then you hospitalized older people. They essentially got a physical while they're in the hospital.
MR. SMITH: There was none of that day surgery stuff.
MR. PICKETT: No. Everybody was admitted.
MR. SMITH: You had surgery. You were in there overnight because that hospital was making the money on you being there.
MR. PICKETT: Right, and if you had a headache, you were liable to get a brain scan, an EEG, and skull X-rays. You'd get all sorts of things. Anything that could be possibly related, you got the testing for it.
MR. SMITH: They might have been 95 percent sure, but we could always get them to 99 percent sure.
MR. PICKETT: Right.
MR. SMITH: This practice was putting money in the hospital's budgets.
MR. PICKETT: That's right, but when DRGs were adopted by Medicare (and I'm not saying it's bad), referring physicians and clinicians had to become more selective in the studies that they ordered, whereas it used to be, what I call, “carte blanche.” Prior to DRGs, they could pretty much order anything they wanted, and these tests would be performed on the patients, and sometimes the tests would show something that another test wouldn't. However, when DRGs came along, there was a limited amount of money. For instance, I specifically remember that brain scans were frequently performed in order to rule out a tumor or whatever, but when CT came along, places that would do 10 scans a day did none. They might do one or two a month. It was so dramatic. I just can't express it enough. As a company, we saw a 30% reduction in the need for nuclear medicine services in the matter of three months.
MR. SMITH: It had a dramatic impact on the technologists at that time, and one of the things you learned was if you had an opportunity (and this is still going on today) to learn more than one field, you would learn it. Multimodality imaging—that was some protection from getting laid off, because I remember very rich hospitals of today were laying people off back then.
And I remember one person in particular got laid off in one of the facilities. The next place he went he got an opportunity to learn MRI, and he jumped on it. He figured that he had better make himself so valuable they couldn't get rid of him.
MR. PICKETT: I became registered in 1984 in abdomen and OB/GYN ultrasound. Other technologists I knew were seeking multiple modality registrations, too. I didn't go to school for it. I learned it on the job because I had, as I said, 30% more time available to me after three months because we just weren't doing as much nuclear medicine. We were really struggling, so I and a few others in our company went to a two-week school to learn the basics, but the rest of it was with radiologists teaching us, and I got my ultrasound registry. Also, there were a number of nuclear techs who had previously been X-ray techs, and they went back to doing both.
MR. SMITH: It is amazing that it does run in such cycles because as big an impact as DRGs had in the mid '80s, managed care had the same effect in the early to mid '90s. Managed Care just changed the way you approached medicine and it had a dramatic impact on the techs. With managed care physicians could not make as much money in the hospitals as they were used to, and it looked like every doctor bought an outpatient imaging center. The volume of nuclear medicine studies performed in these centers was less. Many of my graduates over the years have learned CT and MRI because, I'm sure that during the downtime, when they were at an outpatient imaging center, they went over to their buddies that were doing CT and MRI and picked it up.
MR. SMITH: It's just amazing what a technologist needs to know now with PET/CT and SPECT/CT. I thought one of the nice things about getting into nuclear medicine at the time was that I could always reason stuff out, and I believe that in nuclear medicine a lot of what you did you can think through logically. I didn't have that great a memory, and said, Well, I don't want to be an X-ray tech because you get one shot, and you need to know everything about the structure of the body. That’s changed now: we're putting functional imaging right on top of the anatomical image. You've got to know your anatomy. It's more detailed than we ever had to know.
MR. METZGER: I’m ignorant. What exactly did DRG’s do? How did they change things?
MR. PICKETT: Here’s an example of what DRGs did: If a patient was submitted with pneumonia, the government said, “The diagnosis code for a patient admitted with pneumonia shows that we will only pay this many dollars to the hospital.” It might be $2,000 or $2,500. This was the limit the government would pay for a Medicare patient in the hospital—those over 65 years old.
Now, there were involved ways that if they needed a bone scan while they were there that they could change the DRG code, but prior to DRGs, whatever procedures were done, whatever the patient's hospital bill, Medicare paid a per-procedure or per-item or per-exam price. They reimbursed the hospital X amount of dollars for each and every thing that was done, almost without any kind of accountability of why did you perform that test. The government did this to control costs. The cost of healthcare was spiraling up because, as Glenn said earlier, essentially the hospitals were generating significant dollars from nuclear medicine procedures.
MR. SMITH: And the only way that you could survive in nuclear medicine was to show that your studies actually saved money. The only way that we could exist back then was to show that nuclear medicine was efficient and that you had the best test for that particular patient problem. And just as today, you had to promote it in your hospitals, to the referring physicians. You could have the best tests in the world, but if you didn't promote it by showing how it would also save money and help the hospital, it wasn't doing to be done.
MR. METZGER: So DRGs were the government's cost-cutting effort, and managed care is the insurer's cost-cutting effort. Right?
MR. SMITH: Right.
MR. METZGER: Interesting, so in view of both cost-cutting efforts, do you think that a nuclear medicine technologist would be wise to become multi-skilled, a registered X-ray tech, for example?
MR. SMITH: I think it was a safeguard.
MR. PICKETT: There you go. I think it increased some technologists’ ability to stay in the field. I think the field lost some people who were not multi-skilled. Others, like myself, adapted by getting registered in another modality.
MR. SMITH: Managed Care just dramatically changed the way you looked at things. You had to move the patients in and move them out. That's the way the hospitals were making the money.
MR. PICKETT: Being multi-skilled has not been popular amongst true nuclear medicine professionals.
MR. SMITH: Right.
MR. PICKETT: It tends to take on a negative connotation. I think that there are a number of us that have done it, for instance, in ultrasound, X-ray or whatever. I think knowing other modalities helps you tremendously in the field of nuclear medicine, but I think that, like anything else, if you can stay true nuclear medicine and not be multi-skilled, well, I hate to say it but you're probably going to be a better nuclear medicine technologist. I can’t be sure that's true, but—
MR. SMITH: It's hard to know so much about both fields. It’s hard to be an expert in two fields.
MR. PICKETT: Right.
MR. SMITH: The good thing about PET/CT and SPECT/CT is that you don’t have to go completely through CT school. The professional societies are now working together because there are just not enough individuals that know radiography and nuclear medicine, and there are a lot fewer that know CT and nuclear medicine. They have developed special training modules where if you're a nuclear med tech, you can learn certain aspects of CT that are specific to fusion technology and after successfully completing a test you can receive an advanced certificate.
MR. PICKETT: I maintain my registry in ultrasound, but I would have to bet that the technologist who may not even have passed their registry yet is doing it every day is going to be better at it than I am even though I passed my registry and kept my education up.
I want to be very clear that while it adds value to know the other things, I still think that the true nuclear medicine professional who is dedicated just to nuclear medicine is going to be able to function better than one who is trying to do a little bit of everything.
That doesn't mean that the ones who are doing a little bit of everything are doing a bad job. It's just that -- that if you have the luxury of focusing on one modality, I think that you probably are going to be better at it.
MR. METZGER: All right. Well, we discussed a little bit about memorable people you've come into contact with. Is there anyone else you can think of from Chapter leadership that you'd like to give us some insight regarding, a story or two?
MR. SMITH: I remember hanging out with Brad Pounds and Art Hall after meetings. This was always a lot of fun. Although in ’86 Brad and I were on a plane together and missed the no-hitter Mike Scott pitched to clinch the division for the Astros that year.
In ’94 Art, Brad and I were together for an SNM meeting in Toronto. The Rockets were playing in their first championship. There was a Houston contingent there, and we were sneaking out to find TVs because we wanted to see the Rockets win that year. After they won, a bunch of us from Houston were running through the streets yelling. I’m sure we looked pretty crazy, and, you know, nobody else in the city got it. We even tried to turn over a car, but it just didn't work.
That’s just an example of the value of friendships we made through the Chapter. Some of the first educators I met were Sharon Ward and Martha Pickett. It was good to meet them. Those were the early years back when I was with the school, and it was interesting to meet with people that were doing the same thing that I was doing. There are just not that many nuclear medicine schools, and it was great to meet them. They were great supporters.
MR. PICKETT: I think that leads into that next question you mentioned regarding what’s special or unique about the Southwestern Chapter.
It’s the relationships.
MR. SMITH: Yeah, it's the lifelong friendships.
MR. PICKETT: It's a five-state area that's as small as your backyard in one way but yet is as big as a quarter of the United States in another. The people are really close. Brad Pounds, you know—
MR. SMITH: We lost a good one when he left our region.
MR. PICKETT: You know, he knew my wife's name. His wife was a principal at a high school. You just knew things about people, and you were close. Even though you weren't next door to each other, you just knew about people, and I personally think that's what’s unique about the Southwestern Chapter.
MR. SMITH: I think that's it too. Lifelong friendships that you make with people; that you keep in touch.
MR. PICKETT: The meetings are always great, but it's the people you meet that make Chapter participation meaningful.
MR. SMITH: Right, it's just like church. It’s not just a building—it’s the people that are in it, and it's the same way with the Chapter. It's the people.
MR. METZGER: Alright. Well, irrespective of Chapter involvement, what are some highlights of your own practice of nuclear medicine?
MR. SMITH: I'd have to sum it up in one word and that's education. For 24 years, I've been program director of the Houston Community College's program here teaching technologists. And I can tell you, if I'm feeling down or overwhelmed, there's nothing like the high that you can get by going into one of the area hospitals’ nuclear medicine departments and see techs you’ve trained. My partner, Rene Hyder, and I, we can go into any Houston area hospital and 75 percent or 100 percent of the department is made up of people that we had the honor of training at some point in time. It’s just a super feeling to visit and know that these are not just your graduates. And they weren't just your students, but they’ve become lifelong friends.
And it's just as big a thrill to watch people that you train get into the leadership roles and run the meetings. We're looking at doing some continuing education here in the future, and you're bringing back experts in the area that were the people in your program who have gone on to do more than we've done here, and that's just exciting.
And watching the field grow. Just being there in the early years when you're on a rectilinear scanner—then you were excited if you could see ribs in a bone scan. Then compare that to what we see today. It's just incredible the changes that we've seen over time. It's just amazing, and it still seems like we're in the infancy in nuclear medicine because there's just so much more that I can just see coming down the pike.
But I think that's it—the relationships with the students over the many, many years. And it’s developing friendships with people at the local, Chapter, and National meetings so you can call them and ask for their input or advice. John still sends his company’s reps to our job fair. I saw David Moates down here last week. That’s an important part of my job—getting students employment when they finish. And having friends like John, whose company will send representatives down here to talk with the students and get to know them, that just does it for me.
MR. PICKETT: For me, the highlight is providing nuclear medicine services in rural Texas. We're actually in Illinois now. We're in a lot of areas, and for the most part I would say 75 percent of our nuclear medicine studies are performed in hospitals or facilities with under a hundred beds—in a rural setting. Some facilities are as small as 25 beds. We may go through once a week, but it allows even the small-town doctor to get bone scans or HIDA scans—even cardiac SPECT. We've got some places we may only go two or three times a week, but it allows the patients not to have to travel to a large metropolitan area and fight the traffic and everything. We still can provide those services out in a more remote or a rural setting.
And it's very rewarding to work with these people. I guess it makes you appreciate the rural lifestyle to some extent also. Our technologists get to know folks. They have repeat customers you might say—individuals who return for bone scan checkups every year, for example. It’s a different experience from the majority of Chapter members who work in a more urban setting. For our company, it has been very rewarding to provide these services in the small town, more rural setting.
MR. SMITH: It's amazing, John, what they've got to know in a small town. My mom was hospitalized during the New Year's holiday. She was in Memorial Hospital in New Braunfels, and I visited the nuclear medicine department and spoke with the tech, and it was amazing what he had to do as compared to what we do in the city. The closest pharmacy to him is two hours away in San Antonio, so he’s making up every single kit. I think the only thing he didn't have was a generator. He gets bulk Tech, and he's making up everything.
John, your company has to provide a lot of support to the individuals that are out there too. Right? They're not just on islands.
MR. PICKETT: Right, and that’s why it’s our company’s philosophy and practice to use the same equipment across in all the hospitals that we use. We use X brand, which allows our techs to be really good with one piece of equipment, and they can work in any of the hospitals that we serve. Also, if a tech has a problem in one place, they can actually just pick up the phone and call one of our other techs.
Well, last question: What do you think is the future direction of nuclear medicine? Looking ahead, what do you see?
MR. SMITH: I think it may depend on where you’re working. In the urban areas and the hospitals that have the money that they have, you look ahead and see PET/CT and SPECT/CT. There's a lot of different training going on.
I think nuclear medicine specifically will be in good shape. I think it's always been up to the radiopharmaceutical companies to come up products that will perform well. I think therapy is also a big area in the future. We're still in the infancy of that. I know that Dr. Podoloff thinks that therapy someday will surpass the imaging side of nuclear medicine. That’s difficult for me to conceive of, but he's with M.D. Anderson, and they're doing a lot of research; there are a lot of things going on.
What do you think, John?
MR. PICKETT: I think PET/CT is going to become more and more important. PET has transformed nuclear medicine so quickly. First we had true PET just by itself and now PET/CT fusion within a matter of a couple of years? Normally, you buy equipment with longevity of five to seven years. However, folks that bought PET by itself may be disappointed because PET/CT has come along, and it's almost eclipsed true PET. And that's not just in the urban setting. I think even the guys that have PET on trailers and are coming to the Wacos and that size market. PET/CT is going to the thing. When offered, people are jumping to PET/CT. I went to RSNA this year, and GE told me that of the 84 systems they placed worldwide this last year, not one of them was dedicated PET. They were all PET/CT combinations.
MR. SMITH: PET’s sensitivity is just amazing. One speaker illustrated the value of PET by mentioning how physicians couldn’t determine if a patient had cancer—it was indeterminate. And the options were do either CT or MRI in six months or do PET now. PET is able to pick it up that much earlier. It's expensive, but what it saves and what it can do in hospital care is going to be even more amazing in the future.
MR. PICKETT: I think it's really exciting the way CMS is going to reimburse for it. They've changed, and they've added a whole lot of the indications and they're actually developing a database in which physicians will submit what kind of value they get out of PET/CT for what particular cancers or what particular study they're doing. CMS then, in a very innovative move, will plan to reimburse PET based on the value it is to these particular studies. This is something brand new, and it gives me a lot of hope that PET may be able to become a lot more available outside of large centers. As more PET/CT scanners are sold, the price will come down. I know that the price has come down in the last two years tremendously, and they've already got some of PET/CT scanners on the refurbish market from GE.
MR. SMITH: And I think PET and PET/CT will provide significant savings regarding health care costs. For example, if the PET picks up some things, it may not be beneficial for the patient to undergo surgery because they see tumors in other areas of the body. They were going to cut off a leg, but they found tumors in others areas of the body. Of course, that is bad for the patient, but look what it is saving as far as the mental anguish of going through an amputation. And on the business side, PET helps cut costs because you are able to direct the health care delivery more efficiently. This actually saves money and does a better job for the patient.